So why is a patient’s chance of surviving at some hospitals, such as the one where Dahart works, significantly higher than at others?
“That’s what’s troubling,” says Paul Chan, a leading cardiac arrest researcher at Saint Luke’s Mid America Heart Institute, Kansas City, who works closely with Nallamothu. “That’s what gives people the head-scratching moment.”
The effort to restart someone’s heart is a physical one, requiring chest compressions that mimic the pump, pump, pump of the heart, pushing oxygen-rich blood to the brain.
The compressions must be fast – roughly 110 a minute, nearly two per second – using straight arms, pushing down 5 to 6 cm on the patient’s breastbone. To help maintain those rapid compressions, Dahart will sometimes encourage others in the team to sing the staccato rhythm of the Bee Gees’ Stayin’ Alive.
The exertion can leave a clinician drenched in sweat, their triceps burning from the effort. Occasionally the patient’s ribs will crack beneath the force. If the patient has just had open-heart surgery, Dahart says she might wrap a clipboard with a towel, so she can more evenly distribute the pressure of the compressions across the chest, reducing the possibility of re-fracturing the breastbone.
Dahart, part of a cadre of ICU nurses dedicated to cardiac arrest at her hospital, always ensures that another colleague is poised to step in after two minutes.
“As you fatigue, two minutes is a long time,” Dahart says. “If you’re doing it correctly, you are going to beg for mercy after about a minute and a quarter.”
With each passing minute that a patient’s heart isn’t beating, damage to brain tissue, and thus long-term disability or death, is increasingly likely.
When Olga Rafidi arrived at an emergency room in Ohio, she was walked to the room where clinicians had been working to restore her 48-year-old sister’s heartbeat during a series of arrests. They had been trying for 90 minutes.
Olga describes the next few minutes like it happened yesterday, not six years ago. The nurse, she says, was exhausted. “She could barely talk.” And the room looked like a “war zone”. Plastic, paper, gloves and other medical trash were strewn everywhere, the doctor and other clinicians soaked by their own sweat.
Her sister, Rima Rafidi-Kern, was tied to tubes, not moving.
“She looked like if you would take a piece of meat, like a steak, and beat it, and how it gets thin and big. That’s how she looked. She looked wider and thinner. There was no muscle tone. And she was grey, literally grey.”
But the clinicians had regained a pulse. They raced with Rima to the ICU. Olga took off her shoes and followed them, running.
Created by Wellcome
The heart-stopping reality of cardiac arrest
By Charlotte Huff
Cardiac arrests are usually deadly, even when they happen in well-equipped, well-staffed hospitals. So researchers are trying to understand how best to help more people survive and recover.
Tweet (opens in a new tab) Share by email (opens an email client) Share on Facebook (opens in a new tab) Share link
“Wherever you are, you run.” The next cardiac arrest could strike a patient dozing in their hospital bed, lying in the catheterisation lab or walking down some hallway in between.
One time, Amy Dahart – an intensive care unit nurse at Mary Washington Hospital in Virginia – was part of a cardiac arrest team in a freight elevator, moving a patient from a general ward to the ICU, when the man’s heart stopped. Dahart recounts how another nurse “just launched right up onto that bed, straddled the guy, and started doing compressions… we wheeled him right into the ICU, right through the doors without missing a beat”.
When a cardiac arrest happens, says cardiologist Brahmajee Nallamothu, “that individual automatically becomes the sickest person in the whole hospital”.
Each year millions of people worldwide will suffer an arrest, their hearts abruptly ceasing to beat. Many of these arrests happen in hospital – in the US, roughly one-third – and yet little attention has focused on how to improve treatment of these. A review of 92 randomised controlled studies conducted worldwide, most of them outside of the US, found that just 11 covered the treatment of in-hospital arrests.
Nallamothu, who practises at the University of Michigan, is part of a cohort of cardiologists and other researchers that are trying to dig into the nuts and bolts of in-hospital arrests, in large part to solve an unsettling conundrum. For years now, the science of how to bring someone back from essentially the dead hasn’t changed much: chest compressions, an electrical jolt from a defibrillator if the heart rhythm is considered shockable, making sure the patient is on a ventilator or has some breathing assistance, along with administering fluids and a few key drugs.
So why is a patient’s chance of surviving at some hospitals, such as the one where Dahart works, significantly higher than at others?
“That’s what’s troubling,” says Paul Chan, a leading cardiac arrest researcher at Saint Luke’s Mid America Heart Institute, Kansas City, who works closely with Nallamothu. “That’s what gives people the head-scratching moment.”
© Merijn Hos for Mosaic
The effort to restart someone’s heart is a physical one, requiring chest compressions that mimic the pump, pump, pump of the heart, pushing oxygen-rich blood to the brain.
The compressions must be fast – roughly 110 a minute, nearly two per second – using straight arms, pushing down 5 to 6 cm on the patient’s breastbone. To help maintain those rapid compressions, Dahart will sometimes encourage others in the team to sing the staccato rhythm of the Bee Gees’ Stayin’ Alive.
The exertion can leave a clinician drenched in sweat, their triceps burning from the effort. Occasionally the patient’s ribs will crack beneath the force. If the patient has just had open-heart surgery, Dahart says she might wrap a clipboard with a towel, so she can more evenly distribute the pressure of the compressions across the chest, reducing the possibility of re-fracturing the breastbone.
Dahart, part of a cadre of ICU nurses dedicated to cardiac arrest at her hospital, always ensures that another colleague is poised to step in after two minutes.
“As you fatigue, two minutes is a long time,” Dahart says. “If you’re doing it correctly, you are going to beg for mercy after about a minute and a quarter.”
With each passing minute that a patient’s heart isn’t beating, damage to brain tissue, and thus long-term disability or death, is increasingly likely.
When Olga Rafidi arrived at an emergency room in Ohio, she was walked to the room where clinicians had been working to restore her 48-year-old sister’s heartbeat during a series of arrests. They had been trying for 90 minutes.
Olga describes the next few minutes like it happened yesterday, not six years ago. The nurse, she says, was exhausted. “She could barely talk.” And the room looked like a “war zone”. Plastic, paper, gloves and other medical trash were strewn everywhere, the doctor and other clinicians soaked by their own sweat.
Her sister, Rima Rafidi-Kern, was tied to tubes, not moving.
“She looked like if you would take a piece of meat, like a steak, and beat it, and how it gets thin and big. That’s how she looked. She looked wider and thinner. There was no muscle tone. And she was grey, literally grey.”
But the clinicians had regained a pulse. They raced with Rima to the ICU. Olga took off her shoes and followed them, running.
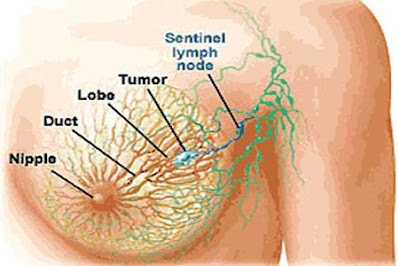
While the heart itself is a muscle, it’s electricity that drives the thumping rhythm of its four chambers, two upper (atria) and two lower (ventricles).
Every heartbeat begins with the body’s natural pacemaker, called the sinus node, which produces an electrical impulse that travels first across the two upper chambers. The atria then contract, pushing blood into the ventricles below. From there, blood is pushed – again driven by electrical impulses – from the ventricles to the lungs, the brain and the rest of the body.
A cardiac arrest is different from a heart attack, which occurs when blood flow is blocked or reduced to an area of the heart, and nearby tissue begins to die. An arrest may follow a heart attack, but the cause is some type of disruption to the heart’s electrical system. It’s immediately life-threatening.
Sometimes the result is a total lack of electrical activity – known medically as asystole and more commonly as flatlining. This is extremely dangerous and hard to treat.
Or the patient might develop ventricular fibrillation, sometimes called VF or V-fib, where the electrical impulses become disorganised and the lower chambers quiver uselessly, unable to pump blood.
VF is considered shockable, potentially able to be righted with a defibrillator – that whining charging sound and the shout of “Clear!” that we hear in medical dramas.
But the reality of cardiac arrest differs from what’s depicted on screen. In a 1996 study that looked at 97 television drama episodes involving 60 CPR (cardiopulmonary resuscitation) attempts (in hospitals and elsewhere), three-quarters of the fictional patients survived, at least in the short term. That can influence our ideas about recovery rates.
A more recent study, published in 2015, looked at the beliefs of family members and other decision makers for ICU patients. It found that nearly three-quarters of them thought that the chance of surviving an arrest exceeded 75 per cent.
The true post-arrest odds, albeit improving, are grimmer. One analysis, involving 24 studies of in-hospital cardiac arrest, found that the chance of leaving the hospital alive averaged about 15 per cent.
Neither does what’s depicted on the screen fully reflect the actual resuscitation experience. Trying to restart someone’s heart is a messy and, in some respects, undignified process, full of beeping machines, ventilators and other paraphernalia. Much of the patient’s skin is left exposed. The room is crowded with clinicians.
And the fictional finale to CPR – survival or death – is less clear-cut than screenwriters would have us believe. Medical dramas typically don’t show patients who regain a pulse but are then a shadow of their former selves. Slightly more than a quarter of in-hospital arrest survivors will live with some degree of brain damage, according to a US study that looked at nearly 85,000 patients from 2000 to 2009. At worst, a survivor might be severely brain-damaged, indefinitely tied to a ventilator.
Fictional patients, says registered nurse Mary Mancini, “come back so nice and clean”.
Patients who are already in the hospital when they have their attack – whether the emergency room or elsewhere – benefit from having doctors, nurses and equipment mere steps away. But they are often already quite ill, whether they’ve been coping with heart failure for years or have recently developed a severe condition, such as sepsis.
For some patients, an arrest might be the final “pathway towards death,” says Brahmajee Nallamothu. For instance, just 7 per cent of patients with advanced cancer survive an in-hospital arrest, according to one analysis.
But the notable variations in survival between hospitals offer some hope, Nallamothu says, that more lives might be saved if hospitals with below-average survival rates adopted some of the strategies of those with better survival rates.
Tony Williams was one of the lucky ones. He was undergoing minor elective surgery in 2018 to remove some large cysts from his back and shoulder, and shortly after the anaesthesia began, his heart stopped.
“It was completely unexpected,” says Tony, who’s 63 and from Herefordshire in England. Tony’s heart had gone into VF, the electrical signals firing in a rapid and disorganised fashion. Three minutes and several shocks later, his heart had been restarted.
Thump. Thump. Thump.
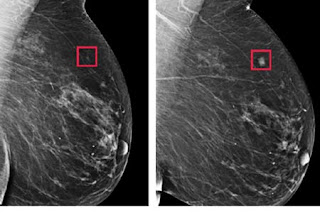
Despite what’s portrayed in the popular media, though, defibrillation is not commonly part of resuscitation. Only one out of five cardiac arrests can benefit from an electric shock.
For this minority of patients, their chance of surviving to leave the hospital are roughly double that of the other four-fifths, according to US registry data. But speed is vital: the sooner you start getting shocked, the better your odds. One study found that nearly one-third of defibrillations started more than two minutes after arrest.
And, throughout the process, continuous chest compressions are vital. “Compressions replace your heartbeat,” says David Heegeman, an emergency physician at Marshfield Medical Center in Wisconsin, which also has been studied by Nallamothu and others for its above-average survival rates. “If your compressions stop, you have no blood flow to the brain.”
When Heegeman analysed cardiac arrests at his hospital some years ago, he realised that compressions sometimes stopped for as long as 30 seconds, such as when the patient’s pulse was checked. Now any pauses are as short as possible, ideally just five seconds to check for a pulse, or to step back right before the next shock is delivered.
While CPR and defibrillation are going on, doctors and other clinicians are striving to figure out what triggered the arrest. It could be a heart attack or a severe condition like sepsis or a toxic exposure, among other possibilities.
Tony’s arrest was caused, he later learned, by an out-of-the-blue anaphylactic reaction to a type of antibiotic he was given during the surgery. He stayed in the ICU in a medically induced coma for several days afterwards. His shaken anaesthesiologist came by to visit him after he was transferred out of intensive care.
“He said, ‘I just would love to shake the hand of the man who survived that, because we didn’t give you much chance.’”
Survival has been improving, at least in the US, based on data coming out of a voluntary registry of hospitals set up two decades ago by the American Heart Association. By 2009, 22 per cent of patients survived to hospital discharge, up from 14 per cent in 2000.
Those strides, though, may not reflect US hospitals overall. Even today, just under 10 per cent of US hospitals participate in the registry, notes Paul Chan, a cardiologist at Saint Luke’s in Missouri. “We may be capturing the best-case scenario.”
Databases and registries of in-hospital cardiac arrests have been launched in other countries in recent years, including in Japan and the UK. But the US registry has one of the longest track records, yielding numerous studies and insights.
For instance, slightly more than half of these arrests occur at night or the weekend. But your shot at survival then is markedly lower, likely in large part because there are fewer staff around.
The ongoing research has exposed a fundamental truth. Your chance of walking away from an in-hospital arrest varies significantly depending upon which hospital you happen to collapse in – even among the roughly 10 per cent of hospitals that participate in the Heart Association’s quality improvement registry.
One analysis, which sorted 468 hospitals from the registry into ten groups based on survival, found that 12 per cent of patients survived in the worst-performing group versus 23 per cent in the top group. Even among similar types of hospitals, such as academic ones or rural ones, there were wide variations in survival rates.
In recent years, Chan, Nallamothu and other researchers have conducted interviews and onsite visits at hospitals with above-average results, including the hospitals where Dahart and Heegeman work.
Increasingly, they’re realising that resuscitation is a team sport that can only be pulled off if the members have been extensively trained, for example with surprise drills, and if they know their precise roles as soon as they arrive.
“I use the analogy sometimes of an orchestra trying to play a beautiful song but they have never practised together,” says Heegeman. “How could you pull that off?”
Add to that the enormous time pressures – to perform perfectly, instantaneously. Compared with treating a heart attack, where the goal is to open that blocked vessel within the first hour, the crux of cardiac arrest treatment ideally should be completed within a far tighter time frame, Chan says. “It’s not 60 minutes, it’s 2 minutes.”
Hospitals with better survival results often have dedicated teams, with members like Dahart who can drop whatever they are doing and race to a code, as cardiac arrests are known in medical parlance. “I just disappear – I don’t even explain,” she says.
Dahart, a nurse for nearly three decades, says that being part of this team is something that she was born to do. “I love codes. I’m not going to lie. I love the adrenaline.” The team, which handles other crises as well, works closely with doctors, respiratory therapists and numerous other clinicians.
But ICU nurses are the team’s core. They debrief after a resuscitation attempt about what went right and what didn’t. Dahart is among those who educate other clinicians about signs that a patient could be imminently vulnerable to an arrest, ideally so the patient can be moved to the ICU before it happens.
When Heegeman started working to improve cardiac arrest survival rates more than a decade ago, he got push-back from some clinicians, who said they already knew how to resuscitate someone. While their clinical skills were strong, Heegeman quickly realised that people needed to practise more as a team, so crucial time wasn’t squandered.
For example, a clinician might arrive to a call but then wait for a leader to assign their role. Sometimes there could be confusion, with two people told to get a defibrillator while another task was left undone. Or too many clinicians could flood the area, making it noisy and difficult to manoeuvre in an already high-pressure crisis.
At his Wisconsin hospital, these days code team members at the start of each shift are assigned colourful lanyards with their cardiac arrest roles on it for that day, whether that’s respiratory therapist or CPR or lab work. So when a code is called, they can pitch in immediately and know everyone’s responsibility. “You don’t even have to say a word and the whole thing is getting done,” says Heegeman.
Rima Rafidi-Kern’s neurologist was pessimistic, given the 90 minutes it had taken to restore a steady pulse. He told her family that she had less than a 1 per cent chance of waking up, Olga says. And, as Olga recounts it, he said that if by some miracle she would wake up, she would likely have overwhelming brain damage.
feeling a sense of crossing into heaven. But as she came to, connected to the ventilator with her mother sitting nearby, she became temporarily disoriented. She saw what seemed to be the mirage of her father, with his arm wrapped around her mother.
Family members took shifts at Rima’s bedside, never leaving her alone. Her twin sister flew in. Priests visited, praying at her bedside. As they were approaching the fifth day after the arrest, Olga says, the family were feeling increasing pressure to make decisions on whether to let Rima go. Then she began to stir, her eyes opening. She tried to mouth words around the ventilator tube that snaked from her mouth: “What happened?”
On social media, cardiac arrest survivors swap stories about memory loss, the number of minutes they were deprived of oxygen and whether they recall any out-of-body experiences. Rima doesn’t remember seeing any light or feeling a sense of crossing into heaven. But as she came to, connected to the ventilator with her mother sitting nearby, she became temporarily disoriented. She saw what seemed to be the mirage of her father, with his arm wrapped around her mother.
Rima reached out to touch her mother’s face. Was she really there in the room? Despite her disorientation, she knew her dad had died some years before
In the weeks after her arrest, Rima learned to live with a few compression-related fractures, discomfort that she gladly accepted as the cost of a second chance at life. Doctors later determined that the anaesthesia from her back surgery had stressed her heart, which already had an undiagnosed blockage.
Olga keeps coming back to what the first doctor told her, the one who started compressions after Rima collapsed in front of him in the emergency room. Normally they would have stopped after about half an hour, he said, as the heart monitor showed a flatline. But the doctor swore he could feel the thread of a pulse. So they continued.
In the years since, Rima has spent a total of roughly six months in two inpatient rehabilitation facilities, working on her memory skills, language and how to handle daily tasks. She needed to use a walker at first, and then a quad cane. Her grown son moved back in to help her for several years.
These days she’s back to living independently, but she acknowledges that it’s more difficult for her to learn new things. She used to love to read, but has difficulty following a book, “especially if it has a lot of characters”.
As for Tony Williams, when he first left the hospital he struggled to walk and dress himself, and he has only recently returned to work full-time as a construction site manager. Initially, he dwelled a lot on his near miss with death. “There was a feeling, especially in the initial stages, you go to sleep and in the back of the mind you’re thinking, ‘Are you going to wake up?’”
With more people surviving cardiac arrests, researchers are trying to get a better sense of what happens after they leave the hospital. Some patients need more support after they return home, says Mary Mancini, who is based at the University of Texas at Arlington and is one of the founders of the American Heart Association’s registry. “They had a truly life-altering event. They were dead. And we brought them back.”
Written by Charlotte Huff

.webp)
.webp)
.webp)
.webp)
.webp)








.webp)
.webp)
.webp)
.webp)

.webp)


.webp)
